How is the NFL concussion protocol supposed to work?
9:27 AM CT
The NFL's concussion protocol, authored and administered jointly with the NFL Players Association, has come under fire in 2017. The most recent criticism came this week, when
Houston Texans quarterback
Tom Savage returned to Sunday's game against the
San Francisco 49ers after
suffering a hit to the head so severe that he displayed apparent signs of what's known as the "fencing response," a classic indication of a brain injury that includes twitching hands.
Known formally as the "Game Day Concussion Diagnosis and Management Protocol,"
the policy in theory should prevent such health-threatening returns to play. That hasn't always been the case this season, as Savage is one of a handful of players who have remained in a game after a hit that was later identified to have caused a concussion.
Here's how the protocol is supposed to work:
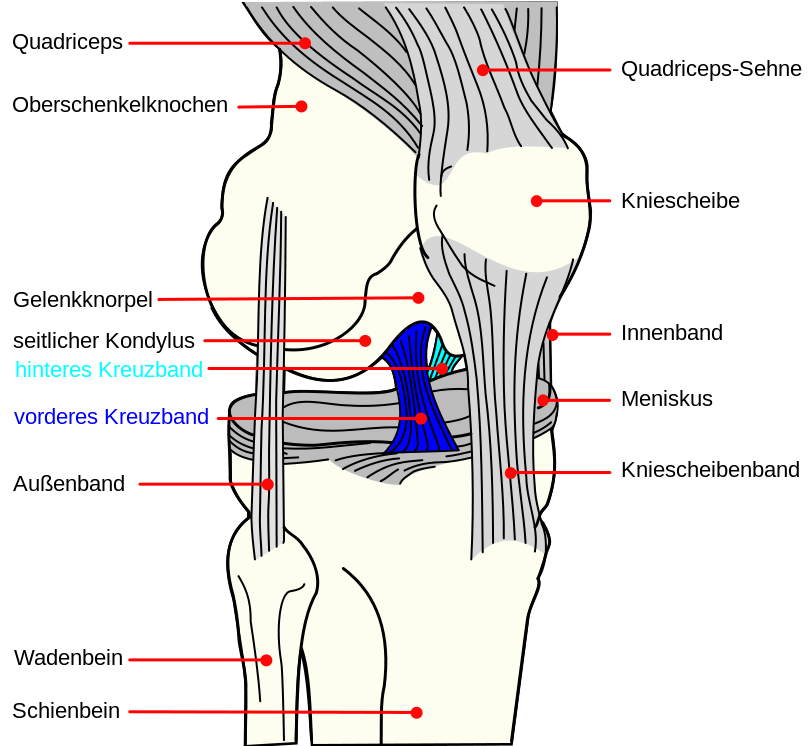
Wait ... can we further clarify 'fencing response'?
Yes. Sometimes a concussion can induce the victim's arms to lock in an odd position, similar to a competing fencer: one arm at the side and the other extended outward. In Savage's case, both arms were extended. Regardless, it is considered a clear indication of brain trauma.
OK, thanks. So let's start from the beginning. How does the policy work on game day?
It begins with the positioning of four independent and dedicated medical professionals. Two certified athletic trainers (ATCs) sit in a booth above field level, acting as "spotters" equipped with video playback gear and a dedicated radio connection with the sidelines. Each team is also assigned an unaffiliated neurological consultant (UNC), who works alongside the team doctor.
'Unaffiliated'?
Yes. The point is to include a medical specialist who doesn't have a stake in the outcome of the game.
Does the NFL have video equipment on the sideline as well?
Yes. Because sideline views can be blocked, each UNC has access to video replays. According to the policy, they can "review the game film on the sidelines to obtain information on particular plays involving possible injury." This equipment is reserved for the medical staff, because football employees are barred from seeing replays on the sideline.
Who is responsible for initiating the process?
Players are encouraged to self-report, and
the team doctor has ultimate responsibility for care. But the ATC spotters in the booth have the authority to call a medical timeout if they identify a player with symptoms. The referee also is asked to send players to the sideline if they see a player displaying symptoms.
REST OF THE STORY
************************
Simply, for those saying that O'Brien should have seen his QB respond as concussed by video sideline film review, O'Brien as a coach does not have access to review sideline video film.